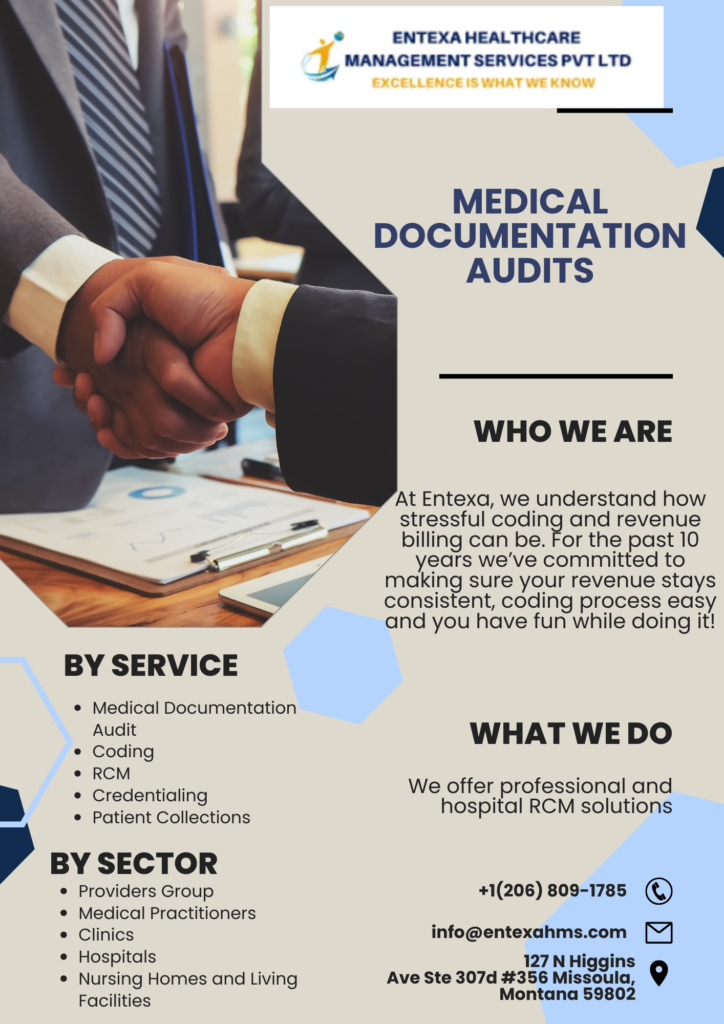
Continuation of our blog posted on September 29 on Medical Documentation Audits by Entexa Healthcare Management Services LLC.
“Coding accuracy” in the context of medical documentation audits by Entexa refers to the precision and correctness of the medical codes assigned to patient diagnoses and procedures in healthcare records. These codes are typically part of the medical coding and billing process, and they play a crucial role in the reimbursement of healthcare services by insurance companies and government healthcare programs like Medicare and Medicaid.
Here’s a breakdown of what “coding accuracy” entails in medical documentation audits:
- Correct Code Assignment: The primary goal of medical coding is to accurately represent the patient’s medical condition and the services provided. Coders must ensure that the codes assigned to diagnoses (ICD-10 codes) and procedures (CPT or HCPCS codes) align with the information documented in the patient’s medical record. Any discrepancies or errors in code assignment can lead to claim denials, underpayment, or even legal consequences.
- Adherence to Coding Guidelines: Medical coders must follow established coding guidelines and conventions, such as those outlined by the American Health Information Management Association (AHIMA) and the American Academy of Professional Coders (AAPC). These guidelines provide specific rules for code selection based on the clinical information available.
- Documentation Support: Coders should rely on the documentation provided by healthcare providers to justify the code selections. If the documentation is insufficient or unclear, they may need to seek clarification from the treating physician to ensure accurate code assignment.
- Compliance with Regulatory Changes: Medical coding is subject to periodic updates and revisions. Coders must stay up-to-date with changes in coding systems, guidelines, and regulations to ensure compliance. Failure to do so can result in coding errors.
- Quality Assurance and Audits: Medical billing companies often conduct internal audits or hire external auditors to review the accuracy of coding. These audits assess whether codes have been assigned correctly, whether coding guidelines have been followed, and whether there are opportunities for improvement in the coding process.
- Education and Training: Continuous education and training of medical coders are essential to maintain coding accuracy. This includes staying informed about the latest coding updates, attending coding workshops, and participating in coding certification programs.
- Reimbursement and Revenue Cycle: Accurate coding has a direct impact on the reimbursement rates for healthcare services. Errors in coding can result in delayed or reduced payments, affecting the revenue cycle of healthcare organizations.
Conclusion
In summary, “coding accuracy” in medical documentation audits by Entexa Healthcare Management Services LLC is all about ensuring that the codes assigned to patient diagnoses and procedures are correct, compliant with guidelines, supported by documentation, and up-to-date with regulatory changes. Accurate coding is critical for proper reimbursement, compliance, and the overall financial health of healthcare providers and organizations.